

While this performance certainly challenges the health system to rethink its focus, perhaps more confronting is the growing body of evidence about significant health and health care disparities based on race, ethnicity, income, zip code, education and other social determinants ( 8). In the landmark Mirror, Mirror International Comparison report done by the Commonwealth Fund, the United States ranked last on performance overall, and ranked last or near last on the Access, Administrative Efficiency, Equity, and Health Care Outcomes domains ( 7). Despite enormous spending on health care per capita, in fact spending more per capita than all other nations in the Organization for Economic Cooperation and Development combined, the United States has staggering and disappointing outcomes- ranking 28 th out of 34 countries in life expectancy, 33 rd in infant mortality and 1 st in poverty ( 5, 6). The health system in the United States is one of the most inequitable when compared to peer developed nations.

The notion that global improvements in quality and delivery of care would improve health disparities and achieve health equity is explicitly false ( 4). However, what became apparent was that a stringent focus on checking the boxes to the Quadruple Aim was insufficient, in and of itself, to reduce health disparities. In fact, the addition of this 4 th aim effectively eclipsed the other aims, because optimization of the initial Triple Aim was now considered impossible without the additional focus on clinician and workforce wellness, resilience and satisfaction.
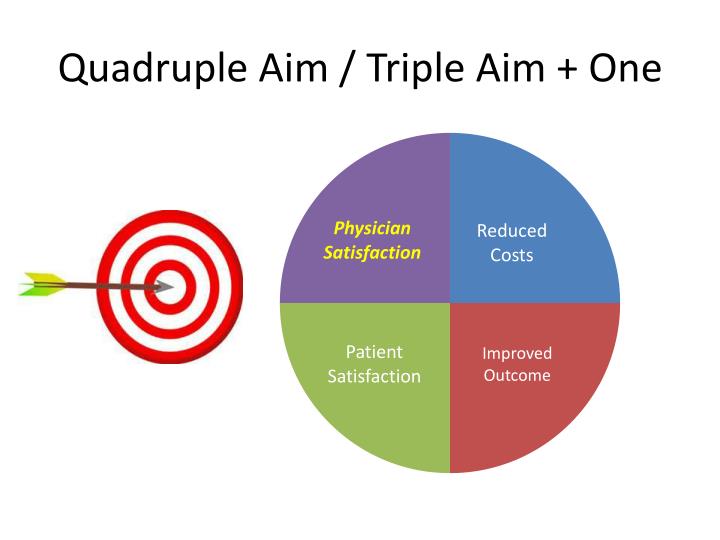
Immediately after and further catalyzed by emerging literature on the enormous financial, clinical and workforce impact of clinician burnout ( 3), evolving clinical settings focused on population health and national alternative payment models for advancing primary care delivery in new ways, and the true north for optimal health system performance was codified-it was now reflected in the Quadruple Aim. Berwick ( 2), an early pioneer of quality improvement in health systems and healthcare, the Quadruple Aim expanded the goals of enhancing patient experience, reducing cost and optimizing population health to include improvements to the work-life and experience of clinicians and care teams that provide care to patients. Building off of the Triple Aim articulated by Dr. Bodenheimer and Sinsky introduced the Quadruple Aim into our health system improvement lexicon ( 1). Email: 09 July 2020 Accepted: 30 October 2020 Published: 25 June 2021. Chair and Professor, Department of Family and Community Medicine The Ohio State University College of Medicine, Columbus, OH, USA.


 0 kommentar(er)
0 kommentar(er)
